- Lyme Disease
- Herxing & Lyme Disease

Herxing & Lyme Disease
Articles
- Brain Fog
- Chronic Fatigue
- Headaches
- Joint Pain
- Lyme Disease
- Muscle Aches
- Skin Rashes/Disorders
Herxing & Lyme Disease
What is a Herx Reaction?
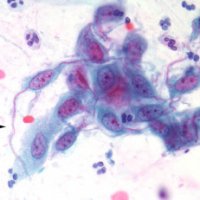
The Jarisch-Herxheimer reaction, often referred to as a Herx reaction or herxing. Herxing can occur when treating bacterial infections such as Lyme disease. This inflammatory response happens when bacteria like the Lyme disease spirochete are killed off rapidly by antibiotic treatment, causing the release of endotoxins into the body. Herx symptoms are sometimes referred to as a die off reaction after patients start antibiotic treatment for Lyme disease.
Jarisch Herxheimer Reaction
The Jarisch-Herxheimer reaction was first observed in 1895 by German dermatologist Adolf Jarisch in syphilis patients with skin lesions being treated with mercury. It involves worsening symptoms shortly after initiation of antibiotic treatment for spirochetal infections. Syphilis bacteria is a type of spirochete, which is in the same family as the Borrelia species which causes Lyme Disease.
The worsening of Lyme disease symptoms after antibiotic treatment can be attributed to the immune system's inflammatory response to the dying Lyme bacteria and the release of lipoproteins from the cell walls of the killed bacteria.
What Causes a Herx Reaction in Lyme Disease?
A Herx reaction is caused by the die-off of bacteria like the Lyme disease spirochete. As antibiotics start killing the infecting bacteria, the bacteria can release toxins and endotoxins like lipoproteins and lipopolysaccharides. All of which can be very inflammatory to the immune system. These toxins trigger the release of inflammatory cytokines like tumor necrosis factor alpha (TNF-α), which are signaling molecules that facilitate communication between cells during immune responses and inflammation. The massive release of cytokines results in flu-like symptoms and inflammatory effects.
Symptoms of a Herx Reaction
Common symptoms of a Herx reaction in Lyme patients include:
- Fever, chills, and excessive sweating
- Headache, lightheadedness, and severe brain fog
- Overwhelming fatigue and weakness
- Intensified muscle and joint pain
- Swollen lymph nodes
- Spreading skin rashes and lesions
- Changes in blood pressure

Severe Herx Reaction
The severity of the reaction depends on the spirochete load in the Lyme patient prior to antibiotic treatments. Reactions may range from mildly uncomfortable to severe and extreme, possibly requiring hospitalization in life-threatening cases. Some patients may never experience herx reactions.
Good Herx vs. Severe Herx
Mild to moderate Herx reactions are considered a “good” sign by doctors, indicating the antibiotic treatment is working effectively to kill off the Lyme bacteria infection. However, severe Herx reactions can be dangerous, causing extreme symptoms of cytokine release that may require medical intervention. Severe herxing often point to excessive bacterial die-off and too high of an initial dosage of antibiotics when starting treatment. It's up to the physician to change medications or dosages depending on the amount of herxing in response to the treatment.
How Common is a Herxing during antibiotic treatment?
Herx reactions frequently occur in 30-40% of Lyme disease patients starting antibiotic treatment like doxycycline or amoxicillin [1]. The sudden die-off of the Lyme Borrelia burgdorferi spirochete triggers excess inflammatory cytokine symptoms and a massive inflammatory cascade leading to acute flu-like symptoms. Slowing the pace of Lyme bacterial die off can help reduce the intensity of the reaction.
Herx Reactions vs. Other Treatment Symptoms and Lyme Disease Symptoms
It’s important for doctors to distinguish a Herx reaction from other Lyme disease symptoms and adverse reactions to medication like allergic reactions. Allergies to medication can cause hives, rash, facial swelling, wheezing, and other symptoms absent in a Herx response. Herx reactions usually resolve after some time, while allergic reactions persist until the medication is stopped. Many Lyme disease symptoms will also feel worse during a herxheimer reaction.
Cytokines: The Good and The Bad
While the spike in inflammatory cytokines causes a Herx reaction’s miserable symptoms, cytokine release is a necessary part of the immune system's response to eliminate Lyme bacteria. Cytokines stimulate white blood cells and antibodies to attack and eliminate the sources of infection. With time and steady dosing under the care of a Lyme literate doctor, the immune system adapts to avoid overreacting to dying bacteria.
Herx Reactions and Bartonellosis
Like Lyme disease, Herx reactions can occur when antibiotics are started for associated infections like Bartonella, which are often transmitted by the same tick bite as Lyme [2]. Herx reactions likely point to simultaneous antibiotic-induced die-off of both Lyme and Bartonella bacteria in coinfected patients.
Nrf2 Signals Production of Antioxidants
The Nrf2 protein is emerging as a key player in potentially reducing Herx severity in Lyme patients. Nrf2 controls the production of antioxidants that clear reactive oxidizing agents generated during the cytokine release storm in a Herx reaction [3]. Boosting Nrf2 may help lessen the intensity of inflammatory Herx responses to Lyme antibiotic treatment.
In summary, the Jarisch-Herxheimer or “herx” reaction is a common inflammatory response as Lyme bacteria are rapidly killed off by antibiotic treatment like doxycycline. Milder forms point to effective antibiotic treatment, while severe reactions require modifying or slowing down the antibiotic regimen. With proper monitoring and adjustment, the short-term misery of a herx should lead to the long-term gain of reducing chronic Lyme infections.
References:
[1] Butler, T. (2017). The Jarisch–Herxheimer Reaction After Antibiotic Treatment of Spirochetal Infections: A Review of Recent Cases and Our Understanding of Pathogenesis. The American journal of tropical medicine and hygiene, 96(1), 46–52. [2] Lantos, P.M. (2015). Chronic Lyme disease. Infectious disease clinics of North America, 29(2), 325–340. [3] Wadhwa, N., Jain, S., Talegaonkar, S., Jain, A. K., Ahire, M., Gilhotra, R., Khar, R. K., & Ahmed, F. J. (2019). Cytokines: The Good and the Bad in Alzheimer's Disease. International journal of pharmaceutics, 564, 302–313.
-
{{#owner}}
-
{{#url}}
{{#avatarSrc}}
{{name}} {{/url}} {{^url}} {{#avatar}} {{& avatar}} {{/avatar}} {{name}} {{/url}} - {{/owner}} {{#created}}
- {{created}} {{/created}}